Module VI
Implant therapy in the functional zone and peri-implantitis
Summary:
It is hard to imagine modern dental treatment concepts without the use of implants. Unfortunately, a significant portion of patients are at risk of biological complications such as peri-implant mucositis and peri-implantitis. Critical analysis of the solutions and innovations in dental implantology is of particular importance concerning possible long-term complications. In this context, thorough planning of tooth replacement using dental implants is necessary, especially in patients with coexisting periodontal disease and other risk factors for peri-implant disease.
During this module, we break down all the elements that condition the stable position of bone with dental implants. We focus on selecting the optimal implant system, intraoperative procedures, characteristics of peri-implant hard and soft tissue, as well as designing and performing prosthetic restorations. We also discuss in detail the indications and techniques for augmenting peri-implant soft tissue in various clinical scenarios. We will present digital technologies that allow implant treatment to be precise and predictable.
Contents:
- Biology of peri-implant tissue
- Selection of an implant system
- Importance of supracrestal soft tissue thickness
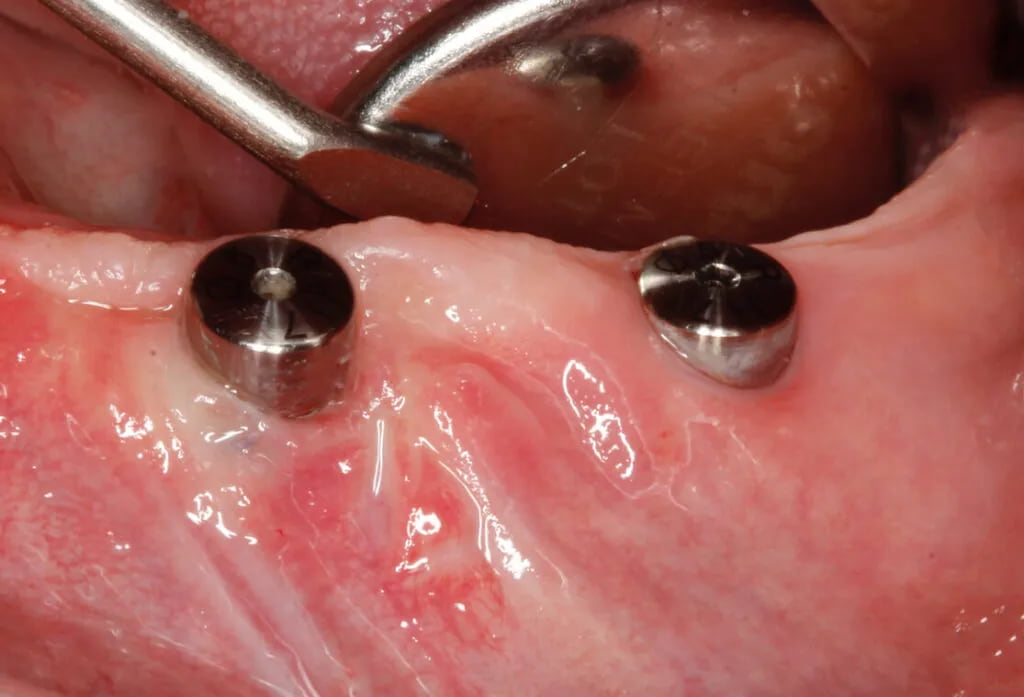
- Assessment and significance of keratinized tissue surrounding implants
- Implant placement and loading protocols
- Guided implant placement
- Implant treatment protocol for patients with periodontal disease
- The increase of keratinized tissue height around implants with free gingival grafts (FGG)
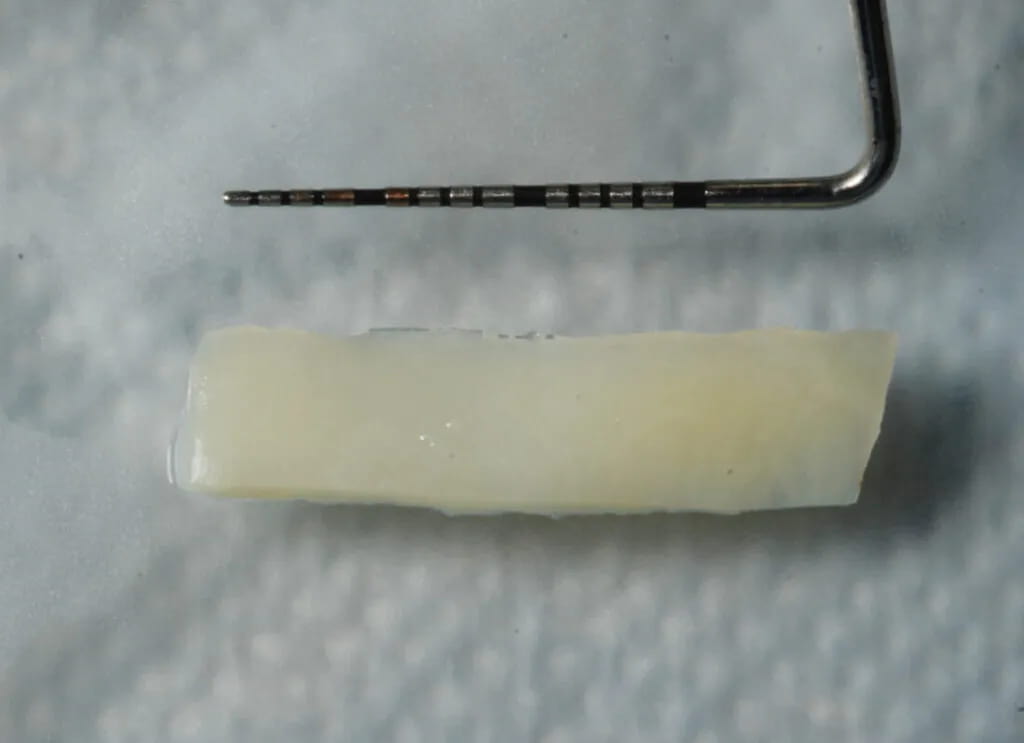
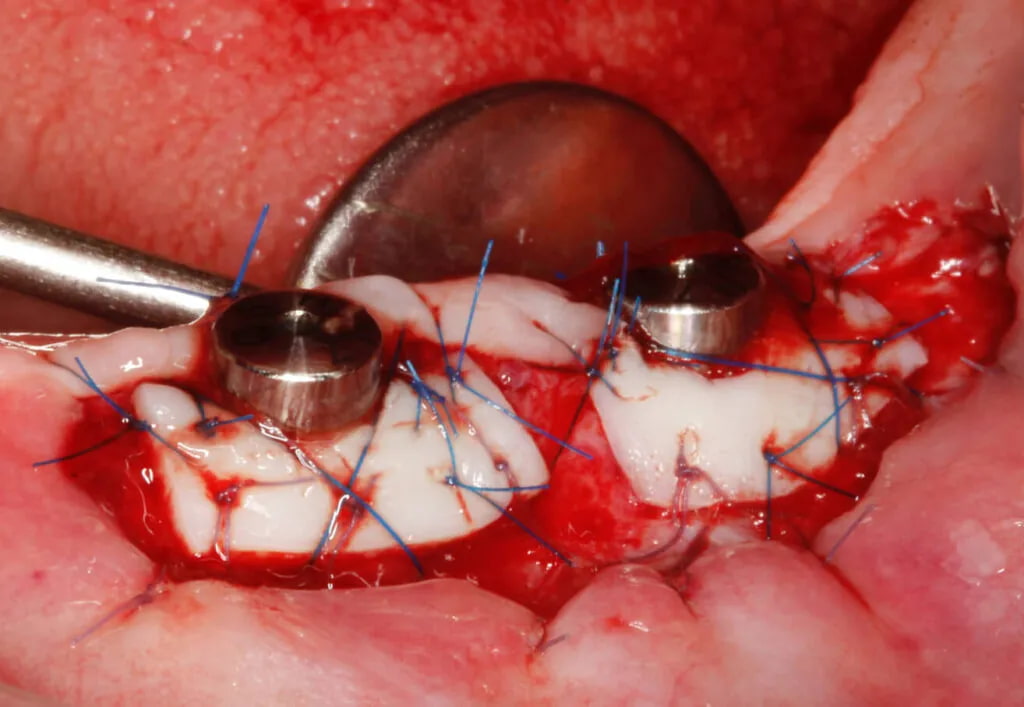
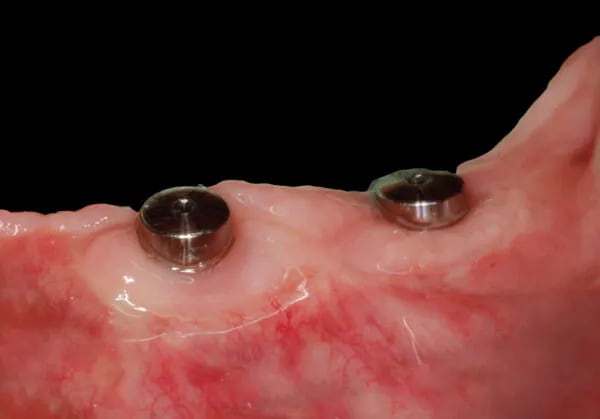
- Soft tissue augmentation with subepithelial connective tissue grafts (SCTG) to increase peri-implant soft tissue volume
- Soft tissue augmentation with soft tissue substitutes to increase peri-implant soft tissue volume
- Prosthetic aspects determining stable bone remodeling around implants: critical and subcritical profiles, prosthodontic material choice
- Peri-implantitis: etiology, diagnostics, treatment protocols, and factors limiting the effectiveness of surgical treatment
Hands-on training::
- Treatment planning using bone-level implants
- Harvesting a subepithelial connective tissue graft (SCTG) using the de-epithelialization technique
- Placement of a bone-level implant with SCTG to augment peri-implant soft tissue volume
- Harvesting a free gingival graft (FGG)
- Placement of a bone-level implant with FGG to increase keratinized tissue height
- Placement of bone-level implants on models using surgical guides, bone remodeling around the coronal aspect of the implant, selecting the healing abutment, selecting the cover screw
- Peri-implant soft tissue augmentation using a collagen matrix